Gender
There was a marked gender disparity amongst the Epsom cluster patients, as for example in the Horton hospital in 1922, only 187 of the 1605 patients were men. This preponderance of women in psychiatric institutions was not unusual – a similar pattern pertained nationally throughout the nineteenth and twentieth centuries, and these characteristics we repeated within European and North American settings. In this time period, highly codified social restraints existed around how women ought to behave, and a refusal to abide by these societal conventions and gendered norms might be interpreted as signs of mental instability. It is telling that phrases as such ‘noisy’, ‘quarrelsome’, ‘aggressive’ and ‘slovenly’ were used as highly gendered descriptions of temperament and character for female patients, alongside detailed observation of appearance and physiognomy, in case books outlining presentation to the hospital.
Within the Victorian period women, as the ‘weaker sex’, were generally held to be more susceptible to disorders of the mind. Physiological differences that purportedly affected their mental health were menstruation, childbearing, aging and menopause. On arrival in the asylums, doctors would take details about female patient’s menstruation, such as the age at which they attained puberty, and the length of their cycle. Until 1980, ‘hysteria’ was considered to be a legitimate medical and psychiatric condition listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM). Symptoms included anxiety, amnesia, paralysis and hallucinations – which have now been replaced or differentiated through other diagnoses. Women were also often sectioned due to postnatal depression.
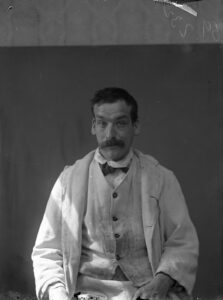
One illness that more often affected men was ‘shell shock’, which we would likely now call post-traumatic stress disorder (PTSD). Between 1918 and 1927, the St Ebba’s Epileptic Colony became Ewell War Hospital, which was dedicated to the treatment of men physically and psychologically affected by the war. ‘Shell shock’ was not widely used as a diagnosis, and doctors could interpret soldiers’ symptoms as physical or mental, leading to a variety of diagnoses. Often, these men were diagnosed with head injuries rather than mental illness. This is likely because mental illness was seen as a sign of weakness incompatible with martial masculinity. Ideas around mental health, such as hysteria being a feminine propensity and insanity more likely for the morally depraved, came to be challenged, and research on shell shock increasingly identified the intertwining of mental and physical presentations. Outside of wartime, St Ebba’s historically had a greater number of male patients than the rest of the Epsom cluster hospitals, as diagnoses of epilepsy encompassed mostly comparable numbers of men and women – though case book descriptions of the effects of this disability continued to highly gendered across the early-to-mid-twentieth century.